Anti-diabetic drugs
The video sessions are for a brief overview. You can view them quickly at the beginning and then go through the question answers.
Diabetes mellitus is a multisystemic endocrine-metabolic disorder associated with inadequate or ineffective insulin or both, affecting the metabolism of carbohydrates, proteins, and fats, and is associated with consistently elevated blood sugar levels that lead to accumulation of glycosylated sorbitol and proteins in tissues causing microangiopathy and damage in multiple organs such as brain, kidneys, retina, heart, and liver ; presenting with complaints such as polydipsia, polyphagia, polyuria, tingling-numbness, blurred vision, and weight loss, and may manifest into many possible complications such as premature atherosclerosis, gangrene in the distal limbs. strokes, nephropathy, retinopathy, silent myocardial infarction, somatic as well as autonomic neuropathy, and susceptibility to infections or skin manifestations.
Two forms of anti-diabetic therapy is mostly used.
- Insulin
- Oral anti-diabetic drugs
One must remember that ORAL anti-diabetics are NOT USED DURING PREGNANCY; and the drug of choice to treat diabetes in pregnancy is insulin.
SAQ/Viva
Mention indications for use of insulin.
1. Type 1 diabetes: Insulin Dependent Diabetes Mellitus (IDDM)
2. Young diabetics / Juvenile diabetes / Early onset diabetes
3. Diabetes in Pregnancy, to treat hyperglycemia during labor
4. Complicated or uncontrolled diabetes – eg. Hyperglycemic coma / Diabetic ketoacidosis, Hyperosmolar non-ketotic coma
5. Situations in the patients of diabetes mellitus such as surgery as well as the peri-operative period, and trauma, infection, septicemia or gangrene
6. Post-pancreatectomy diabetes
7. Primary or Secondary Failure to oral antidiabetic drugs
8. Severe intolerance to oral antidiabetic drugs
9. Too asthenic / underweight diabetic patients
SAQ/Viva
Mention indications for oral antidiabetic drugs.
1. Type 2 diabetes meliitus (Non-Insulin Dependent Diabetes Mellitus) (NIDDM)
2. Diabetes of later age (Late-onset / Adult onset / Maturity onset diabetes) (Age more than 35-40 years)
3. Obese diabetics (Usually metformin – a biguanide is invariably used in obese diabetics)
4. Uncomplicated diabetes
SAQ/Viva
Explain mechanism of action of Insulin.
Insulin receptor is an enzyme linked receptor having two subunits – alpha and beta. The beta subunit is associated with the enzyme tyrosine kinase. It phosphorylates the tyrosine residues, which leads to activation of PIP3 Kinase.
This produces translocation of the ATP dependent glucose transport molecules – GLUT 4 and GLUT 1. These molecules produce the transport of glucose across the cells, and the uptake of glucose by the cells
The steps are summarized below:
- Insulin receptor – Enzyme-linked receptor
- Alpha subunit –
- Beta subunit –tyrosine kinase
- It produces Phosphorylation of tyrosine residues –> which produces activation of PIP3 kinase –>
- Translocation of ATP dependent glucose transporters (Glucose transport molecules) – GLUT 4, 1 –>
- —> Glucose transport,and uptake by the cells
SAQ/Viva
Mention pharmacological actions of insulin.
Insulin is extremely important for transport of glucose across the cells and uptake and utilization of glucose by the cells.
It also works for increasing the breakdown of glucose.
It works in order to decrease the breakdown of proteins and fats, so that their conversion into carbohydrates is prevented.
Insulin also increases the protein synthesis.
Actions:
- Insertion of glucose transport molecules in the cell walls
- Increased glucose utilization by the cells, increased glucose uptake by the cells (especially – the major target organs such as adipose tissue, and skeletal muscle)
- Increased glucose breakdown (INCREASED GLYCO-LYSIS)
- Decreased protein and fat conversion into glucose (DECREASED GLUCO-NEO-GENESIS)
- Anti-lipolytic action – DECREASED FAT BREAKDOWN and inhibit their conversion into carbohydrates
- Increased protein synthesis (by increasing amino acid entry into cells)
- Decreased protein breakdown
SAQ/Viva
Mention adverse effects of insulin; and treatment of insulin hypoglycemia.
Adverse effects of Insulin:
1. Hypoglycemia:Insulin favors utilization and breakdown of glucose; so the most important adverse effect of insulin is HYPOGLYCEMIA (decreased blood glucose levels).
Insulin hypoglycemia is precipitated by following factors (In following situations/factors, the insulin hypoglycemia is more likely)
(1) Missing or skipping a meal: If an individual does not eat or eats less than the usual quantity, and takes the same dose of insulin which is prescribed, the blood glucose will obviously become less.
(2) Taking a higher dose of insulin than what is needed: Diabetic individuals are trained for self administration as well as self modification of doses of subcutaneous insulin injection. If an individual takes higher dose, hypoglycemia will be precipitated.
(3) Excess exercise or exertion: With the same amount of insulin dose, if more exercise or exertion is done, then the blood glucose will fall more than expected.
(4) Stress: Severe stress or repeated episodes of stress increases the risk of hypoglycemia.
(5) Children and older individuals are more prone to insulin hypoglycemia.
(6) Impaired renal function/Renal damage makes the hypoglycemia more likely.
Precautions to prevent hypoglycemia: 1. Don’t miss/skip a meal. 2. Avoid dose adjustments without advice. 3. Do controlled exercise ; do not do excess exercise than what is decided. 4. Carry glucose powder (This has most rapid and instantaneous absorption)
Treatment of insulin hypoglycemia: (1) Oral glucose. Try oral glucose first. If severe, and/or no recovery, then – (2) 50% glucose – 20-50 ml INTRAVENOUS. if no recovery, then – (3) Glucagon Injection 0.5-1 mg Intravenous – or – 1 mg subcutanous – or -Intramuscular. (4) Intravenous Corticosteroid – Dexamethasone. (5) Injection epinephrine 0.2 mg subcutaneous
2. Allergic reactions: They are less likely to newer human insulins as they are less antigenic.
3. Local injection site reactions
4. Weight gain and edema
5. Lipoatrophy or lipodystrophy of subcutaneous fat: This also is less likely with human insulins because they are more pure. The problem of lipodystrophy was severe with older / animal insulins.
6. Insulin resistance: Increased requirement of insulin over longer periods of time – Requirement more than 200 units per day. Insulin resistance is less with human insulins.
7. Insulin presbyopia: Change in the lens curvature due to chronic insulin use
8. Neuropathy, morning headaches, disturbed sleep
SAQ/Viva
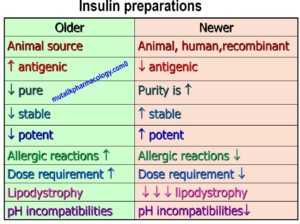
Compare and contrast: Older Insulins and Newer Insulins
Older insulins were mostly obtained from animal source. They were less potent, less stable, less pure, and more antigenic. They did produce more allergic reactions, had more susceptibility to produce lipodystrophy, and more chances of resistance. Newer insulins are mostly human insulins obtained by recombinant DNA technique, and are superior to older/animal insulins in all the above aspects.
SAQ/Viva
Classify insulin preparations with examples.
Insulin preparations are classified based on their duration of action. Initially, they were classified as SHORT/RAPID ACTING (Semi-Lente Insulin), INTERMEDIATE ACTING (Lente Insulin), AND LONG ACTING (Ultra-Lente Insulin). Now we have insulins which are very rapidly acting (Hence called ULTRA RAPID/ULTRA SHORT ACTING), and very long acting (Hence called ULTRA LONG ACTING).
They are shown below with their examples and approximate time for onset of action and duration of action.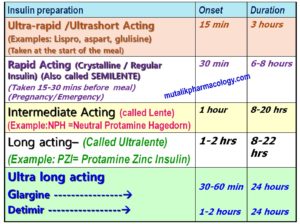
SAQ/Viva
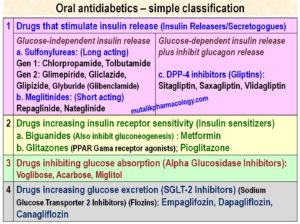
Classify oral antidiabetic drugs with examples.
Oral antidiabetic drugs act by one of the following 4 mechanisms:
- Insulin Releasers: They are also called insulin secretogogues.
-Sulfonylureas and Meglitinides decrease the blood glucose levels, by stimulating the insulin release; and this is irrespective of glucose levels; hence if you haven’t had your enough usual meal, these two groups are more likely to produce hypoglycemia, and the hypoglycemia may be severe. Amongst the two groups, Sulfonylureas are long acting and meglitinides are comparatively shorter acting. (Sulfonylureas and meglitinides block ATP sensitive K channels. This opens up the calcium channels, and leads to insulin release)
-DPP-4 inhibitors (Sitagliptin, Saxagliptin, Vildagliptin): They inhibit the enzyme DPP-4 – Di-Peptidyl Peptidase. (This enzyme inactivates two incretin hormones – Glucagon like peptile – GLP1 and GIP – Glucose dependent Insulinotropic Peptide or Gastric Inhibitory Peptide. These two incretins are supposed to stimulate glucose-dependent insulin release, and inhibit glucagon release). So when DPP-4 is inhibited, incretins accumulate; hence insulin release and glucagon inhibition.
Thus DPP-4 inhibitors indirectly lead to insulin release and glucagon inhibition. However, this insulin release is glucose dependent; hence hypoglycemia is less likely or less dangerous with DPP-4 inhibitors. - Insulin Sensitizers: These increase the sensitivity of the insulin receptors and decrease the insulin resistance. (Biguanides – Metformin; and Glitazones – Pioglitazone)
Biguanides (Metformin) are very important insulin sensitizers, and they do not produce dangerous hypoglycemia like sulfonylureas. (Hence they are euglycemic agents).
Metformin also has important insulin-like actions of inhibiting gluconeogenesis, improving glucose uptake, decreasing glucose output. (It activates AMPK – AMP Activated Protein Kinase), and also decreases glucose absorption.
Metformin also produces nausea, metallic taste, and anorexia – loss of appetite; thus with metformin the patient’s food intake remarkably decreases, and hence metformin produces weight loss. Hence it is preferred in obese diabetics.
The second groups of drugs – Glitazones (Pioglitazone) – are related to perioxisome proliferator activated receptor gene – which regulates the carbohydrate and fat metabolism. They are agonists of PPAR-gama receptors, and hence they increase the sensitivity of the insulin receptor especially in adipose tissue, liver, and skeletal muscle. So they are also insulin sensitizers. - Drugs that inhibit glucose absorption: Alpha glucosidase is an enzyme present in the brush border of small intestine, which is necessary to convert complex sugars into simple sugar. Alpha glucosidase inhibitors (Voglibose, Acarbose, Miglitol) thus inhibit the conversion of complex sugars into glucose, and decrease the glucose absorption from the intestine. Thus less glucose levels achieved this way can decrease the dose requirement of insulin in the patients receiving insulin. Hence Alpha glucosidase inhibitors are said to have insulin-sparing effect.
- Drugs increasing glucose excretion: SGLT-2 (sodium glucose transporter -2 is present in the proximal convoluted tubules of the kidney, and is responsible for glucose reabsorption from kidneys. SGLT-2 Inhibitors (Dapagliflozin, Canagliflozin, and Empagliflozin) inhibit the gluose reabsorption and thus increase its excretion. Hence glucose excretion is increased.
SAQ/Viva
Mention adverse effects of oral antidiabetic drugs.
| N | Group | Adverse Effects |
| 1 | Sulfonylureas | Hypoglycemia, Weight gain,
Cholestatic Jaundice, Disulfiram like effect (Alcohol intolerance), Renal dysfunction, Hepatic dysfunction |
| 2 | Meglitinides | Hypoglycemia, Weight gain, joint pain, liver dysfunction |
| 3 | DPP-4 inhibitors
(gliptins) |
Hypoglycemia,Gastrointestinal discomfort, Allergic reactions – Anaphylaxis, pancreatitis, hepatotoxicity, increased incidence of infections (immune suppression) |
| 3 | Biguanides
(Metformin) |
Weight loss, Anorexia, nausea, metallic taste, loss of appetite, Abdominal discomfort
B12 deficiency, rare lactic acidosis, hepatic dysfunction |
| 4 | Glitazones | Hunger sensation, Fluid retention, Redistribution of fat, Weight gain, Edema, Heart failure, Cardiotoxicity
Liver dysfunction, Enzyme induction, Increased risk of fractures, Bladder carcinoma |
| 5 | Alpha glucosidase inhibitors | Hypoglycemia not corrected by simple sugar/sucrose, Gastrointestinal discomfort, bloating, flatulence, diarrhea, liver dysfunction, renal dysfunction |
| 6 | SGLT-2 inhibitors
(Flozins) |
Hypoglycemia (less than other antidiabetic drugs), Osmotic dieresis, Increased levels of creatitine, Mg, K, Po4 |
SAQ/Viva
Mention principles of treatment of diabetic ketoacidosis/diabetic coma.
- Low dose insulin by continuous intravenous infusion – Started as Regular insulin – 0.1 to 0.2 units/Kg – followed by 0.1 unit/Kg/Hour by intravenous infusion
The rate is doubled if there is no response in 2 hours.
After 4 to 6 hours, if the blood glucose level falls below 300 mg%, then the rate is reduced to 2-3 units per hour. - Intravenous fluids – Normal saline -1 to 2 liters in the first Hour, then 1 liter per hour for next 3 to 4 hours, then 1 liter every 4 hours.
- Glucose and potassium are added to saline infusion when the blood glucose level decreases as much as 250 mg%. (50 grams of glucose and 20 mEq of KCl added to each 1 liter of fluid).
- Potassium Chloride (KCl) – 10-20 mEq/Hour
- Sodium Bicarbonate Intravenous 50 mEq
- Na-K Phosphate 5-10 mmol/Hour
- Antibiotics
- Ventilatory support
The classification is already there. Check. You must have missed it.