Cholinergic Blockers (Anti-Cholinergic Drugs)
Have a look at this video before going to lecture notes.
REMAINING PART OF THIS VIDEO LECTURE CAN BE FOUND IN THE POST OF SKELETAL MUSCLE RELAXANTS.
Anti-cholinergic Drugs or Cholinergic Blockers are the competitive antagonists of acetylcholine at cholinergic receptors. So they could block the muscarinic sites or nicotinic sites.
Muscarinic blockers are Atropine and its selective substitutes.
Nicotinic blockers are the neuromuscular blocking agents (d-tubocurarine, pancuronium or atracurium like drugs), which relax the skeletal muscles.
SAQ/Viva
Classify cholinergic blockers with examples.
1. Muscarinic Blockers (Anti-muscarinic drugs)
(A) Alkaloids: Atropine, Scopolamine (Hyoscine)
(B) Atropine substitutes
- Antispasmodics: Hyoscine Butyl Bromide, Pirenzepine (specific M1 blocker for peptic ulcer), Dicyclomine, Propantheline, Methantheline, Oxyphenonium, Clidinium, Atropine methonitrate, Isopropamide, Pipenzolate methyl bromide
- Urinary tract antispasmodics: Flavoxate, Oxybutinin, Tolterodine, Drotaverine, Propiverine, Solifenacin, Darifenacin
- Bronchial asthma: Ipratropium bromide, Tiotropium bromide
- Mydriatics: Tropicamide, Cyclopentolate, homatropine, Eucatropine
- Pre-anesthetic medication: Glycopyrrolate
- Anti-Parkinson (Drug induced Parkinson): Trihexyphenidyl (Benzhexol), Benztropine, Procyclidine, Biperiden, Orphenadrine
- Anti-Motion Sickness: Hyoscine (Scopolamine) (as chewable tablets and transdermal patch)
- Uterine relaxant: Valethamate
2. Nicotinic Blockers
(A) Skeletal muscle relaxants (Competitive Neuromuscular blocking agents): d-tubocurarine, pancuronium, atracurium
(B) Ganglion blocking agents: Trimethaphan, mecamylamine
SAQ/Viva
Why atropine/glycopyrrolate is used as pre-anesthetic medication?
Atropine/Glycopyrrolate is an anticholinergic drug. It selectively blocks muscarinic receptors, and blocks the actions of acetylcholine, to bring about following effects.
- Prevents reflex vagal bradycardia, cardiac arrest, and hypotension that may be precipitated by various procedures; and increases AV conduction. Prevents vasovagal attack.
- Decreases all exocrine secretions.
- Relaxes all smooth muscles, namely gastrointestinal tract, urinary tract, and bronchial smooth muscle.
- Helps to prevent laryngospasm by decreasing the respiratory secretions
- Prevents cough reflex.
- Decreases gastric hyperacidity and Prevents vomiting.
SAQ/Viva
Mention contraindications to atropine.
- Acute congestive glaucoma
- Chronic obstructive pulmonary diseases (COPD): Bronchial asthma, bronchitis, bronchiactesis, emphysema
- Retention of urine
- Benign prostatic hyperplasia (BPH)/Carcinoma prostate/Bladder calculus
- Extremes of age
SAQ/Viva
Mention adverse effects of atropine.
Atropine is an anticholinergic – muscarinic blocking agent. It blocks the muscarinic receptor sites namely, heart, smooth muscles, exocrine glands, sphincter pupille and ciliary muscle of lens, and it also crosses blood brain barrier. Following are the adverse effects of atropine. Some of the severe adverse effects shall manifest when there is atropine overdose.
- Dryness of mouth
- Retention of urine
- Blurring of vision and photophobia
- Constipation
- Tachycardia, palpitation
- Decreased secretions, dryness of respiratory secretions leading to respiratory discomfort, dryness of skin, dryness of eyes
- Increased intraocular tension and precipitation of glaucoma
- Increased body temperature (Hyperpyrexia) (in overdose)
- Hot, dry, reddish skin
- Disorientation, confusion, convulsions, and coma
- The classical signs of atropine overdose may be described as – Dry as bone, Blind as bat, Red as meat, Hot as iron, Mad as hatter
SAQ/Viva
Why glycopyrrolate is preferred over atropine as pre-anesthetic medication?
Glycopyrrolate is an atropine substitute. It is preferred to atropine as preanesthetic medication for following reasons:
- Less tachycardia than atropine
- Less chances of arrhythmia
- Better control of oropharyngeal secretions
- Maintains more stability of cardiovascular system
- More rapid recovery after anesthesia
SAQ/Viva
Mention the advantages of atropine substitutes.
Atropine is an anticholinergic drug which selectively blocks the muscarinic receptor sites. But it is NOT SELECTIVE WITHIN THE MUSCCARINIC RECEPTOR SITES. so it blocks all the muscarinic receptor sites and hence causes many unwanted effects.
Atropine substitutes are designed to have selective action WITHIN the various muscarinic receptor sites, and hence can be specifically used for particular conditions. In addition, some of them can be used locally – without producing actions on other sites. So the advantages are:
- Selectivity WITHIN the muscarinic receptor sites.
- Specificity of action – e.g. some act predominantly only on GIT, some on urinary tract.
- Least adverse effects on other muscarinic sites on which a particular atropine substitute has less effects
- Availability in the form of preparations used for local effects – e.g. Ipratropium and tiotropium by inhalation in patients with bronchial asthma
- Shorter duration of action than atropine – especially in the eye (e.g, cyclopentolate, tropicamide), where mydriasis and cycloplegia with atropine can last upto a week to produce photophobia and blurring of vision.
SAQ/Viva
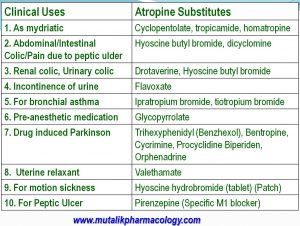
Mention atropine substitutes and their uses.
LAQ/SAQ/viva
Mention the therapeutic uses of atropine explaining its basis of action.
Atropine is an anticholinergic – muscarinic blocking agent. It blocks the muscarinic receptors located at – Heart , Smooth muscles, Exocrine Glands, Sphincter pupilae, Ciliary muscle of lens, and CNS (Central nervous system). It increases AV conduction and leads to some cardiac stimulation; decreases the various secretions, relaxes the gastrointestinal, genitourinary, and bronchial smooth muscle, produces passive mydriasis and cycloplegia, and can increase the intraocular pressure. Its therapeutic uses are based on these actions.
- Organophosphorous compound poisoning: 2-3 mg IV to start with and continued as needed with monitoring of size of pupils and heart rate. (Organosphosphorous compounds are irreversible anti-cholinesterase agents, which inhibit the enzyme choline-esterase and prevent breakdown of acetylcholine. So acetylcholine accumulates; atropine blocks the muscarinic actions of acetylcholine by competitive antagonism)
- Early mushroom poisoning: To reverse the muscarinic actions
- Anti-choline-esterase overdose (Physostigmine poisoning/neostigmine overdose): Overdose by anti-choline-esterase drugs like physostigmine, because atropine blocks their muscarinic actions, and also helps to reverse the central effects because atropine crosses blood brain barrier.
- Pre-anesthetic medication: Because atropine prevents reflex vagal bradycardia, hypotension, and cardiac arrest; decreases secretions; prevents cough reflex, vomiting reflex, and laryngospasm; and relaxes all smooth muscles.
- Sinus bradycardia and AV block: As atropine increases AV conduction
- Digitalis-induced sinus bradycardia and AV block: as atropine increases AV conduction
- By local instillation as a mydriatic and cycloplegic agent in eye conditions and procedures
- As antispasmodic in gastrointestinal, renal, biliary colic and pain of peptic ulcer
- Along with neostigmine/pyridostigmine in myasthenia gravis, to block their muscarinic adverse effects
- Along with neostigmine/edrophonium (to block their muscarinic actions) in treatment of curare poisoning
- In drug-induced Parkinson, to block the cholinergic excess in the basal ganglia, and to help relieve tremors and rigidity
SAQ/Viva
Mention the pharmacological actions of atropine.
Atropine is an anticholinergic – antimuscarinic agent, which selectively and competitively blocks only the muscarinic receptor sites. Its actions are as follows:
- Heart: Stimulation. Decreases vagal tone, Mild tachycardia, palpitation, increased AV conduction
- Smooth muscle: Relaxes gastrointestinal smooth muscle, urinary tract and uterine smooth muscles (called antispasmodic action), and bronchial smooth muscles
- Exocrine glands: Decreases secretions of salivary glands, lacrimal glands, sweat glands, and tracheobronchial respiratory secretions, and gastric hydrochloric acid secretion
- Eye: (a) Paralyzes sphincter pupillae (Circular muscle of iris/constrictor pupillae), which leads to passive contraction of radial muscle of iris, leading to dilation of pupil (Passive mydriasis)(Light reflex is abolished). (b) Paralyzes ciliary muscle of lens, (Cycloplegia) leading to paralysis of accommodation, so that the lens is fixed for far vision. so there is inability to accommodate for near vision. Both actions can lead to blurring of vision and photophobia. (c) Increases intraocular pressure
- CNS: Crosses blood brain barrier. (a) Suppresses tremors and rigidity of Parkinsonism (b) Has anti-motion sickness properties (c) can produce disorientation, confusion (d) Increases the body tempera
Sir plz upload smooth muscle relaxant and local anaesthesia note
Thanks for the feedback. Skeletal muscle relaxants are added. Please check.