Prokinetics and Anti-emetics
Prokinetics are the drugs which stimulate the forward movement of the gastrointestinal tract; whereas Anti-emetics help prevent or stop vomiting.
Since some prokinetics do have predominant action on the upper gastrointestinal tract, such drugs are useful as antiemetics. So some prokinetics are antiemetics.
Antiemetics help prevent or stop vomiting due to various causes. So apart from prokinetics, there are other drugs which are also useful as antiemetics.
SAQ/Viva
What to you mean by Pro-kinetics? Enumerate their actions.
Prokinetics are the drugs which stimulate the movement of the gastrointestinal tract by increasing the frequency or strength of contractions and help move the contents in the upper GI tract still forwards.
The term practially applies more significantly to the drugs which have predominant action on the upper part of the gastrointestinal tract. Some prokinetics exert their action throughout the gastrointestinal tract.
Actions of Prokinetics:
- Stimulate gut motor function
- Promote gastrointestinal transit
- Increase gastro-esophageal sphincter tone (lower esophageal sphincter (LES) tone
- Stimulate gastric emptying by coordinated propulsive movement
- Antiemetic / D2 blocking action
SAQ/Viva
Classify/Mention/Enumerate Prokinetics,with their mechanism of action.
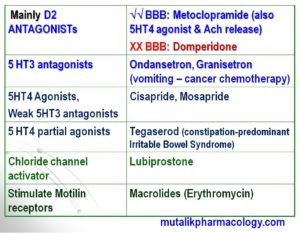
SAQ/Viva
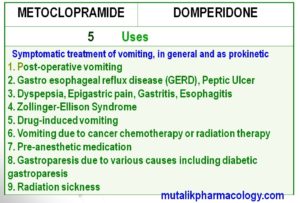
Mention the uses of prokinetic agents.
- Symptomatic treatment of vomiting, in general
- Post-operative vomiting
- Gastro esophageal reflux disease (GERD/GORD)
- Non-ulcer dyspepsia (Bloating, Gastric empyting abnormalities, Epigastric pain)
- Zollinger-Ellison Syndrome
- Gastritis
- Esophagitis
- Peptic ulcer
- Drug-induced / Opioid induced vomiting
- Vomiting due to cancer chemotherapy: Ondansetron
- Vomiting due to radiation therapy
- Pre-anesthetic medication (General anesthesia)
- Gastroparesis due to various causes including diabetic gastroparesis
- Vagotomy
- Constipation-predominant irritable bowel syndrome (Tegaserod)
- Radiation sickness
- Chronic constipation
SAQ/Viva/LAQ
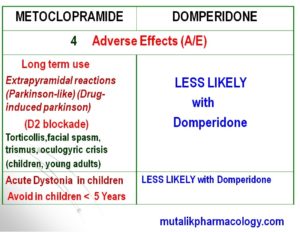
Compare and Contrast: Metoclopramide and Domperidone
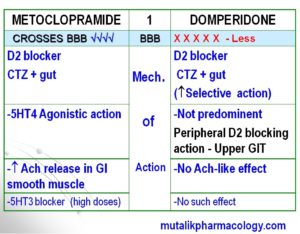
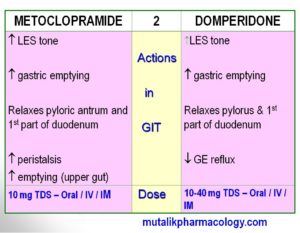
Below are five different items showing the compare and contrast. It includes mechanism of action, actions, doses, adverse effects, and uses of both the drugs. You can make use of these tables to review both drugs simultaneously and understand that –
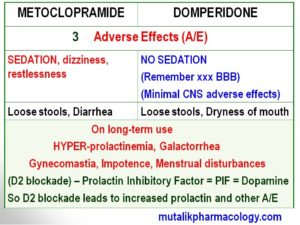
-Both are D2 blockers, but domperidone has less penetration across blood brain barrier (BBB), and is less likely to produce sedation.
-So also Domperidone is less likely to produce Extrapyramidal reactions (Parkinson-like syndrome).
-However, both the drugs have a susceptibility to produce hyperprolactinemia, galactorrhea, impotence, menstrual disturbances, gynecomastia and such related symptoms. (This is because the prolactin-inhibitor-factor – PIF is itself dopamine. So when dopamine gets blocked by these drugs, its inhibition of prolactin inhibitory factor, and in turn leads to hyperprolactinemia and the related symptoms)
-5HT4 agonistic action as well as stimulation of acetylcholine (Ach) release is predominant with metoclopramide; whereas these effects are insignificant with domperidone. Domperidone’s predominant effect is Peripheral D2 blocking action in GIT, and more selective D2 blocking action centrally.
-Both have common uses pertaining to prokinetic action and anti-emetic action in various conditions leading to vomiting.
Study the following tables referring to the above facts shown at different places.
SAQ/Viva
Mention / Classify Antiemetics.
- Prokinetic agents: Metoclopramide, Domperidone, Mosapride, Cisapride, Tegaserod
- 5-HT-3 Antagonists: Ondansetron, Granisetron
- H1 antihistamines: Promethazine chlorotheophyllinate (Avomine), Promethazine Hydrochloride (Phenergan), Doxylamine, Cinnarizine, Cyclizine, Meclizine, Buclizine, Diphenhydramine, Dimenhydrinate
- Anticholinergics: Hyoscine (Scopolamine), Dicyclomine
- Neuroleptics: Chlorpromazine, Prochlorperazine, Haloperidol
- Others: Pyridoxine, Betahistine, Benzodiazepines (Diazepam/Lorazepam), Dexamethasone, Cannabinoids (Nabilone, Dronabinol)
We may also mention antiemetics based on which drugs are more commonly used in which conditions.
| Specific cause of vomiting | Drugs commonly used | |
| 1 | Preanesthetic/Post-op (Post GA) | Promethazine, Ondansetron, Metoclopramide, Domeperidone |
| 2 | Vertigo | Betahistine, Prochlorperazine, Cyclizine, Cinnarizine |
| 3 | Cancer chemotherapy/Radiation | Ondansetron, Granisetron, Dexamethazone, Lorazepam, Diazepam, Nabilone, Dronabinol, Metoclopramide, Domperidone |
| 4 | Pregnancy
10-14 weeks |
Doxylamine, Pyridoxine, Promethazine, Metoclopramide, Domperidone |
| 5 | Motion Sickness | Hyoscine (Scopolamine), Promethazine Chlorotheophyllinate, Promethazine hydrochloride, Cyclizine, Meclizine, Dimenhydrrinate |
| 6 | Drug induced | Metoclopramide, Domperidone, Promethazine |
| 7 | Metoclopramide and Domperidone : Dyspepsia, Bloating, Peptic ulcer, Gastritis, Esophagitis, GERD, Zollinger-Ellison, Pre-op / Post-op vomiting, Drug-induced, Cancer chemotherapy/Radiation, Pregnancy | |
Viva
Which anticancer drugs commonly produce severe vomiting? Why? Which antiemetics are useful to treat cancer chemotherapy induced vomiting?
Anticancer drugs that lead to severe vomiting: Cisplatin, mechlorethamine, dacarbazine, carmustine, cyclophosphamide, adriamycin, carboplatin, asparaginase
Most of the anticancer drugs – especially those mentioned above, produce release of large amounts of 5-HT from enterochromaffin cells in gut mucosa, This stimulates 5HT3 receptors, and therefore there is vomiting.
Therefore the drugs which block the 5HT-3 receptors (5HT-3 antagonists) – (Ondansetron/Granisetron) are more specific in relieving/preventing cancer chemotherapy induced vomiting.
Sir , 5-HT3 antagonist r antiemetic drugs or prokinetic drugs ??
I did not understand the question. They are prokinetics as well as antiemetics.
Thank you sir!
These notes are really very helpful
Read and revise. Watch the videos.