Local anesthetics
Local anesthetics are applied or administered locally and produce loss of all sensations in the area of supply, without affecting the consciousness.
Methods of local anesthesia include surface anesthesia (Topical anesthesia) (mucous membranes/skin), infiltration anesthesia (Field block/nerve block/trunk block/plexus block), spinal anesthesia (subarachnoid space), epidural anesthesia (epidural space), and intravenous regional anesthesia (Bier’s block). Usually the sensations that are lost first are – pain and temperature, and then the other sensations.
Local anesthetics act by blocking the sodium (Na+) channels and blocking the sodium entry, thereby preventing the depolarization, and thus blocking the generation and conduction of nerve impulse.
Special points
- Xylocaine, Lidocaine, Lignocaine are all same ! They are different names of the same drug !
- Surface Anesthesia (Topical Anesthesia) means applying the drugs mainly to mucous membranes by local application (oral cavity – gel, drops – eye , ointment – anal canal)
- Amide-linked local anesthetics (Lidocaine, Prilocaine, Bupivacaine etc) have less chances of producing hypersensitivity reactions.
- Ester-linked local anesthetics (Procaine, chloroprocaine, tetracaine, benzocaine) have more chances of producing hypersensitivy reactions
- Procaine is not used as surface anesthetic. It does not penetrate.
- Local anesthetics are combined with epinephrine (adrenaline) to prolong the duration of action of anesthesia.
- Bupivacaine is one of the longest acting local anesthetics.
- Prilocaine produces Methemoglobinemia.
- Bupivacaine produces Cardiotoxicity.
- Local anesthetic also useful as antiarrhythmic agent: Lidocaine
SAQ/LAQ/Viva
Mention mechanism of action, uses, adverse effects, and salient features of lidocaine.
Lidocaine (Lignocaine/Xylocaine) is the most widely used local anesthetic.
It is an amide-linked, soluble local anesthetic, and is one of the safest local anesthetics, because the chances of hypersensitivity reactions are less.
It is used for all methods of local anesthesia (for all types of blocks).
Mechanism of action: Lidocaine crosses the cell membrane and blocks voltage gated Na+ channels from inside the membrane, and inhibits entry of Na+ ions. So it prevents depolarization of the membrane, and thereby prevents generation and conduction of nerve impulse.
Mechanism of action summarized as:
- Crosses the cell membrane
- Blocks the Voltage gated Na+ channels from inner side of membrane
- Inhibits sodium entry
- Prevents depolarization (Depolarization Block)
- Prevents generation of nerve impulse (Generation Block)
- Prevents conduction of nerve impulse (Conduction Block)
Uses:
- Surface anesthesia (Topical anesthesia) (Mucous membrane – oral cavity, anal canal) (Not used for eye)
- Used with prilocaine,as eutectic mixture-EMLA- for intact skin – venepuncture, skin graft
- Infiltration anesthesia (Field/Nerve/Trunk/Plexus block – suturing of wounds, minor procedures, dental extractions).
- Spinal anesthesia
- Epidural anesthesia
Salient features:
- Fairly rapid onset of action (2 to 5 minutes)
- Fairly long duration of action (60 to 120 minutes)
- Duration of action of anesthesia can be further prolonged by addition of a vasoconstrictor agent like epinephrine.
- Minimal local irritation
- Useful for all types of blocks under all methods of anesthesia.
- Less chances of hypersensitivity reactions (amide linked structure)
- Acts by blocking Na+ channels
- Also useful by INTRAVENOUS route as an ANTIARRHYTHMIC agent (Class IB) for ventricular arrhythmia
- Adverse effects to lidocaine are rare, and include hypotension, cardiac arrest, mental clouding/drowsiness/central nervous system depression, and convulsions.
Lidocaine-Epinephrine combination:
Lidocaine is sometimes combined with epinephrine (1:50,000 or 1:80,000 or 1:100,000 or 1:200,000). The basis for this combination is as follows:
1. Epinephrine stimulates the alpha-1 receptors to constrict the smaller blood vessels, and decreases the rate of entry of lidocaine to systemic circulation; so it remains concentrated locally.
2. So its contact time with nerve fiber increases, and its duration of action gets prolonged. (Epinephrine prolongs the duration of action of lidocaine)
3. Its systemic absorption and systemic toxicity is minimized.
4. Local bleeding is minimized.
The above combination is contraindicated –
- at areas supplied by end arteries (toe tips, finger tips, male sex organ) due to fear of ischemia and necrosis.
- in patients with history of severe hypertension, arrhythmia, angina or other cardiovascular diseases.
SAQ/Viva
Compare and contrast: General anesthetics versus local anesthetics
| Criterion | General anesthetics | Local anesthetics |
| Administration | By a route for systemic action | By a route for local action |
| Acion | Systemic | Local |
| Area affected | Whole body | Area of supply by the blocked nerves/nerve roots |
| Site of action | CNS | Local nerves/nerve roots |
| Usual routes | Intravenous / Inhalation | Local administration-application /instillation / infiltration/ spinal /epidural |
| Consciousness | Lost | Not affected |
| Systemic toxicity | Possible | Minimal expected |
| Central nervous system | Depression | Least affected |
| Cardiovascular function | Depressed | Minimal/least depression |
| Respiratory function | Depressed | Minimal/least depression |
| Used for | Major surgery | Comparatively minor surgeries/procedures and some major surgeries |
| Examples | Intravenous – Thiopental, profofol, etomidate
Inhalation – desflurane, sevoflurane, enflurane, nitrous oxide, halothane, ether, isoflurane |
Lidocaine, Prilocaine, Bupivacaine, Mepivacaine, Ropivacaine, Etidocaine, Dibucaine
Procaine, Chlorprocine, Tetracaine, Benzocaine, Oxethazaine |
LAQ/SAQ/Viva
Classify local anesthetics with examples.

SAQ/Viva
What is surface anesthesia? Give examples.
Surface anesthesia is the local anesthesia to intact or abraded skin or mucous membranes. It is also called Topical Anesthesia.
The local anesthetics for topical use may be available in the form of cream, gel, ointment, liquid, spray, eye drops, ear drops etc.
Drugs which are more lipid soluble drugs, they can cross the membranes easily, and hence they are likely to be good surface anesthetics.
Procaine has poor penetration through the mucous membrane of the eye, hence Procaine is not used as surface anesthetic in the eye.
Examples:
Eye drops – Tonometry, eye surgery – (Tetracaine, Benoxinate, Proparacaine)
Ear drops –
Ointment, creams – Proctoscopy, piles, anal fissure
Spray – Bronchoscopy, Nasal spray
Oral ingestion of suspension for local anesthesia – To relieve pain of peptic ulcer (Oxethazaine used with antacid suspension)
Cream of an Emulsified local anesthetic mixture under occlusive dressing – EMLA for intact skin as an alternative to infiltration anesthesia – Prilocaine and Lidocaine mixure – 2.5 each]
EXAMPLES of topical anesthetics: Benzocaine, Butamben, Dibucaine, Lidocaine, Oxybuprocaine, Pramoxine, Proparacaine, Proxymetacaine, Tetracaine (amethocaine)
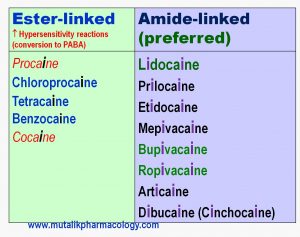
Mention ester linked and amide linked local anesthetics. What is the importance of the structure?
Local anesthetics have an aromatic ring with an intermediate linkage to this ring.
If the intermediate linkage is an ESTER (C=O), then they are called ester-linked local anesthetics. Examples: Procaine, chlorprocaine, tetracaine, benzocaine etc..
If the intermediate linkage to the aromatic ring is an AMIDE (NH-C=O), then they are called amide-linked local anesthetics. Examples: Lidocaine, Bupivacaine, Prilocaine, Etidocaine etc.
Ester linked local anesthetics get broken down to PABA, which is more likely to produce hypersensitivity reactions. So hypersensitivity reactions are more likely with ester-linked local anesthetics. There is also cross reactivity within the ester linked local anesthetics. (It is also interesting that due to the typical way of nomenclature, ester linked local anesthetics have only one “i”s in the spellings of their names).
Amide linked local anesthetics do not get broken down to PABA, and hence are comparatively safer as far as chances of hypersensitivity reactions are concerned. So amide linked local anesthetics are preferred. (It is also notable that due to the way of forming the nomenclature, the amide linked local anesthetics have 2 “i”s in the spelling of their names.)
Look at the spellings of the names of various local anesthetics in the table below:
SAQ/Viva
What is eutectic mixture? Mention its uses.
EM = Emulsified LA – Local anesthetics
EUTECTIC MIXTURE means an Emulsified Mixture of Lidocaine + Prilocaine at room temperature – in the concentration 2.5 % each – available as cream. (Formulations of 2% or 7% each also available)
It is applied on the intact skin (under an occlusive dressing).
It is applied 30-60 minutes before a procedure.
It penetrates the intact skin. It covers the depth upto 5 mm. Local anesthesia lasts for about 1-2 hours.
Uses: It serves as an alternative to infiltration anesthesia for –
- Venepuncture
- Skin graft harvesting
- Intravenous Cannulation
- Minor dermatological procedures
It should not be applied to mucous membranes or abraded skin., because it can get rapidly absorbed and produce systemic toxicity.
SAQ/Viva
Write in brief about spinal anesthesia.
Spinal anesthesia is administered in the subarachnoid space into the cerebrospinal fluid, usually between L3-L4.
It anesthetizes a larger area below umbilicus, without the risks of general anesthesia and without affecting consciousness. it is useful for procedures lasting upto few hours.
Area:Below umbilicus (lower abdomen, perineum, pelvis, lower limbs)
Examples of operations: Lower Segment Cesarean Section, appendicectomy, many orthopedic operations on Lower limbs (e.g. joint replacement), hernia, piles, fissures.
Drugs commonly used for spinal anesthesia: Lidocaine, Bupivacaine, Tetracaine, Procaine.
Complications: Common: Mild Hypotension, bradycardia, nausea, vomiting, back pain, headache. (Hypotension during spinal anesthesia is usually treated with methoxamine, mephenteramine, or ephedrine)
Rare: Nerve injury (cauda equina syndrome – loss of bowel bladder control; radiculopathy), cardiac arrest, severe hypotension, respiratory paralysis, septic meningitis
Contraindications: Severe hypotension, Hypovolemia, Mentally ill or uncooperative patients, Infants and children, Vertebral column abnormalities / pre-existing spinal cord lesions
SAQ/Viva
Write briefly on Epidural Anesthesia
Injection of a local anesthetic drug into epidural space is called Epidural Anesthesia.
It is usually used for anesthesia in the region below umbilicus (lower abdomen, perineum, pelvis, and the lower limbs).
By this method, the anesthesia of longer duration can be achieved by repeated administration of anesthetic drug through the catheter inserted into the epidural space. So also, post-operative analgesia can be obtained by keeping the catheter in the epidural space intact and continuing the drug administration. The commonly used drugs include lidocaine and bupivacaine.
Hence, epidural anesthesia is preferred especially if the procedure is going to last for longer duration.
Sometimes epidural anesthesia is useful for pain relief also after thoracic or upper abdominal surgery.
By this method, the normal delivery can be performed without pain. This is called painless labor. (0.25{2610912583dabb07030bf2cdad608afafcc4beb0908ae67f305141b9a5c99c63} bupivacaine).
As compared to spinal anesthesia, headaches or neurological complications are comparatively less in epidural anesthesia; although the cardiovascular complications may be similar to spinal anesthesia.
SAQ/Viva
Enumerate the local anesthetic drugs used in dentistry.
The following drugs are used commonly in dentistry with or without epinephrine.
- Lidocaine (Xylocaine/Lignocaine)
- Prilocaine
- Articaine
- Mupivacaine
- Bupivacaine
Various concentrations of adrenaline when it is combined with local anesthetics are: 1,50,000, or 1:80,000 or 1:100,000 or 1:200,000.
Depending on the site and extent of injection, the local anesthetics shall produce reversible loss of all sensations in the divisions of mandibular and maxillary branches of trigeminal nerve. They will be useful for periodontal or oral surgery, restorative dentistry, and endodontic treatment.
I used to find pharmacology subject difficult before i started learning from this site.
very helpfull and everything is so easy to grasp.
thank you for such guidance sir.
Yes. The site has come out with great effort and experience. The students should make the best of it.
Sir thank u so much… Its amazing… And it is really helpful
Thanks. Share it with your friends in other MBBS and BDS colleges.
Thank you sir. This is really very helpful…
Please add autacoids- antihistaminics notes asap.
and GIT also.
Thanks. Yes, it is being added.