Cholinergic Drugs- Agonists and Anti-Cholinesterase Agents
Cholinergic Drugs include –
Cholinergic Agonists which DIRECTLY stimulate the cholinergic receptors, and also those which
INDIRECTLY act on this receptor by increasing the amounts of acetylchline (by inhibiting acetylcholine breakdown by the enzyme cholinesterase), hence called Anti-Choline-Esterase Agents (Anti-ChE agents)
SAQ/LAQ/Viva
Enumerate cholinergic receptor sites and briefly indicate the cholinergic actions.
Cholinergic receptor sites or actions are of two types: Muscarinic (M) and Nicotinic (N).
Muscarinic called so because these actions are like muscarine, an alkaloid found in mushroom. Nicotinic called so because these actions were found to be similar to nicotine actions.
To summarize, through the muscarinic sites –
- Acetylcholine controls the heart from excessive stimulation.
- Acetylcholine is needed for contraction of the smooth muscle of GIT, respiratory, and urinary tract.
- Acetylcholine stimulates secretions of exocrine glands including salivary, respiratory, and other secretions.
- Acetylcholine is responsible for contraction of sphincter pupillae leading to constriction of pupils (miosis) and stimulation of ciliary muscle of lens for accommodation.
- Its needed for normal memory function in the brain
- Cholinergic excess in the brain leads to tremors, rigidity, excess salivation.
Muscarinic actions/sites
- Heart: Inhibition – M2
- Smooth muscle: Stimulation (Contraction) (Respiratory, GI, Urinary tract) – M3
- Exocrine glands: Stimulation (secretion) – M3
- Eye: Sphincter Pupillae (Contraction, Miosis) and Ciliary muscle of lens (Accommodation), and decreased intraocular pressure – M3
- CNS
Avoid the complications of remembering which is M1, which is M2 etc, by remembering a simple formula – MOST ARE M3, (except heart and CNS). (So smooth muscle , exocrine glands, and eye – ALL ARE M3).
—HEART IS M2.
—CNS has various types at different sites [Learning/memory is related to M1, Basal ganglia is related to M2, and some other are also M4,M5]
—-Parietal cells of gastric mucosa concerned with gastric HCl secretion are M1.
Now go back to the list of muscarinic receptors given above and confirm the subtypes !
Nicotinic actions/sites
- Skeletal neuromuscular junction (NM)
- Autonomic ganglia (NN)
- Adrenal medulla(NN)
SAQ/LAQ/Viva
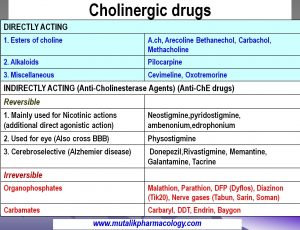
Classify Cholinergic Drugs with examples.
The two main classes are: DIRECTLY ACTING and INDIRECTLY ACTING.
Directly acting drugs stimulate the cholinergic receptor.
Indirectly acting drugs are given this name because they themselves do not directly stimulate the receptor, but act by inhibiting the breakdown of acetylcholine (A,ch) by inhibiting the enzyme choline-esterase, thus acetylcholine accumulates and it stimulates the cholinergic receptors. In other words “Indirectly acting” agents are Anti-Choline-Esterase Drugs (Anti-ChE drugs)
DIRECTLY ACTING
- Esters of choline:A.ch, Arecoline Bethanechol, Carbachol, Methacholine
- Alkaloids: Pilocarpine (Pilocarpus spp. – A south american plant)
- Miscellaneous: Cevimeline, Oxotremorine
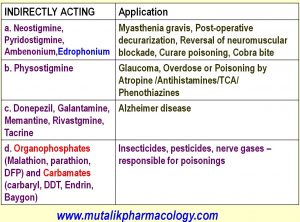
INDIRECTLY ACTING (anti-Choline-Esterase Agents) (Anti-ChE drugs)
I. Reversible:
(a) Mainly used for Nicotinic actions (Have additional direct agonistic properties: Neostigmine,pyridostigmine, ambenonium, edrophonium (Neostigmine also useful in post-operative paralytic ileus and gastric-intestinal-bladder atony).
(b) Acting also on eye and CNS: Physostigmine
(c) Cerebroselective: Donepezil, Rivastigmine, Memantine, Galantamine, Tacrine
II. Irreversible:
(a) Organophosphates (organophosphorous compounds): Malathion, Parathion, DFP (Dyflos),Diazinon (Tik20), Nerve gases (Tabun, Sarin, Soman)
(b) Carbamates: Carbaryl, DDT, Endrin, Baygon
Revise the same in the table form as given below:
Here is another classification which also helps to remember the therapeutic application of the cholinergic drugs.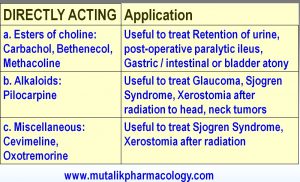
SAQ/Viva
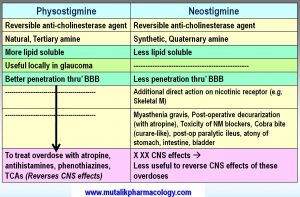
Why physostigmine is used in Atropine overdose?
Atropine is an anticholinergic agent which selectively blocks the muscarinic receptor sites.
Physostigmine is an anti-choline-esterase drug. So –
- It inhibits the enzyme choline-esterase and accumulates acetylcholine at and this acetylcholine gradually displaces atropine competitively from the muscarinic sites, thus reverses the effects of atropine overdose.
- Most importantly, Physostigmine is highly lipid soluble, and hence is able to cross the blood brain barrier and enter the central nervous system, and hence shall be able to reverse the most serious central effects as well as peripheral effects of atropine overdose. (Neostigmine have less penetration in CNS, hence cannot reverse the central effects).
SAQ/Viva
Why neostigmine is preferred to physostigmine in the treatment of myasthenia gravis?
Neostigmine and Physostigmine both are anti-choline-esterase agents.
They prevent the breakdown of acetylcholine by the enzyme choline-eserase, and thus accumulate acetylcholine. Its accumulation at nicotinic receptor is beneficial in myasthenia gravis.
In addition to this, neostigmine has an additional advantage – It has a direct agonistic action on the nicotinic receptor. Thus it directly depolarizes the muscle end plate. Therefore it is more effective than physostigmine.
Morever Neostigmine has minimal penetration across blood brain barrier.
Hence neostigmine is preferred to physostigmine in the management of myasthenia gravis.
SAQ/Viva
Compare and contrast – Physostigmine and Neostigmine
SAQ/Viva
Mention adverse effects of anti-choline-Esterase drugs.
Anti-choline-Esterase drugs act by inhibiting cholinesterase enzyme and accumulating acetylcholine at all muscarnic and nicotinic receptors. So their adverse effects are the effects of excess acetylcholine at these receptor sites. We can derive them as follows: (Please note: The same following will be the manifestations of organophosphorous compound poisoning, because they are anti-chline-esterase drugs !!)
- Heart: (Inhibition):Bradycardia, hypotension, flushing, heart block
- Smooth muscles: (Contraction) (GIT, Respiratory, Urinary tracts): Diarrhea, nausea, vomiting, abdominal cramps/pain, bronchospasm, breathlessness, incontinence of urine, frequency of micturition
- Exocrine glands: (Stimulation of secretions – gastric glands, salivary and sweat glands, respiratory secretions, eye secretions): Hyperacidity, sialorrhea (excess salivation), seborrhea (excess sweating), watering of eyes (increased lacrimal secretions), increased respiratory secretions
- Eye: (Contraction of circular muscle of iris and ciliary muscle of lens): Miosis, blurring of vision, spasm of accommodation, photophobia
- CNS/Skeletal Muscle: Tremors, fasciculations, muscle paralysis
LAQ/SAQViva
Mention the mechanism of action of organophosphates, the manifestations of organophosphorous compound poisoning, and its treatment.
Organophosphorous compounds are irreversible anti-choline-esterase agents. They are used as insecticies/pesticides (Malathion, parathion, DFP, Diazinon, and nerve gases like sarin, soman, tabun).This is one of the most common poisonings because the substances are very commonly used in agriculture and elsewhere, easily available, and less expensive.
The poisoning/overdose may happen due to: -Accidental exposure (ingested mistaking it for some drug, unknowing self ingestion or inhalation by children/adults themselves, inhaled accidentally during spraying) -Intentional exposure (objective of suicide/homicide).
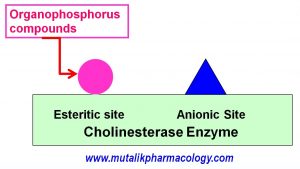
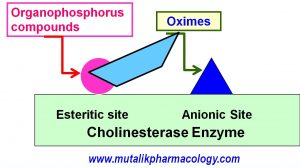
Mechanism of action: Organophosphates combine with the esteritic site on the choline-esterase enzyme, and phosphorylate it. This is a covalent bond which is difficult to reverse. So they are called irreversible anti-choline-esterase agents. Due to this phosphorylation, the choline-esterase enzyme becomes inactive. So the acetylcholine cannot be broken down, and it accumulates at all muscarinic and nicotinic receptor sites.
The manifestations are due to acetylcholine excess, which are as follows:
- Heart:Bradycardia, hypotension, flushing, AV block
- Smooth muscles: (Contraction) (GIT, Respiratory, Urinary tracts): Diarrhea, nausea, vomiting, abdominal cramps/pain, bronchospasm, breathlessness, incontinence of urine, frequency of micturition
- Exocrine glands: (Stimulation of secretions – gastric glands, salivary and sweat glands, respiratory secretions, eye secretions): Hyperacidity, sialorrhea (excess salivation), seborrhea (excess sweating), watering of eyes (increased lacrimal secretions), increased respiratory secretions
- Eye: (Contraction of circular muscle of iris and ciliary muscle of lens): Miosis, blurring of vision, spasm of accommodation, photophobia
- CNS/Skeletal Muscle: Tremors, fasciculations, muscle paralysis
- Acidosis
- Convulsions, loss of consciousness
- Local irritation, pain, and burning in oral cavity
- Local irritant effects like burning, irritation, pain on skin or mucous membranes of eyes and respiratory tract in case of local exposure to these parts.
Treatment:
- Atropine: Anti-cholinergic. Muscarinic blocker. Competes with the accumulated acetylcholine at muscarinic receptor sites, and gradually displaces acetylcholine (Competitive antagonism), and thus reverses the cholinergic effects. Started as 2-3 mg intravenous, and repeated gradually as required with monitoring of -size of pupil (atropine effect is to dilate the pupils), and – heart rate (Benefit of atropine would be indicated by increase in the heart rate). (In severe poisoning, as much as 50 mg or 100 mg or rarely even more atropine may be needed depending on the amount of poison ingested and the severity of poisoning).
- Oximes: Pralidoxime chloride 1-2 mg intravenous. Oximes are called choline-esterase enzyme reactivators or choline-esterase enzyme regenerators. They combine with the anionic site on the choline-esterase enzyme, and de-phosphorylate the esteritic site (remove the phosphorous from the esteritic site), which makes the choline-esterase enzyme free of the organophosphorous compound, which again starts breaking down the accumulated acetylcholine.
- Diazepam or Lorazepam: As anticonvulsant to stop convulsions if they appear.
- Intravenous sodium bicarbonateto combat acidosis
- Keeping the patient in a dark room/less lighted room to avoid more photophobia
- Gastric lavage as soon as the patient is brought in to remove if any unabsorbed poison is still present in the stomach
- Thorough washing of skin and mucous membranes like oral mucous membrane, eyes, nasal mucous membrane, if there is local exposure and irritation.
- Adequate airway maintenance /oxygenation / positive pressure ventilation as needed.