Thrombolytic (Fibrinolytic) Agents
One should not confuse between the three terms – anticoagulants, antiplatelet, and thrombolytic.
Anticoagulants prevent coagulation – are mainly useful in venous thrombosis.
Antiplatelet drugs prevent platelet aggregation – are mainly useful in arterial thrombosis
whereas –
THROMBOLYTICS – dissove the thrombus/clot.
Thrombolytic (Fibrinolytic) agents are the drugs that produce lysis of the thrombus/clot.
These are extremely valuable for producing dissolution of the clot as an emergency in conditions like myocardial infarction and stroke to re-establish the circulation.
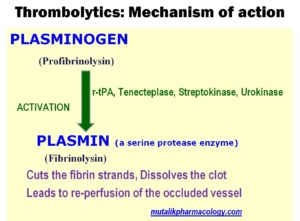
Thrombolytics combine with Plasminogen and activate it to Plasmin.
Plasmin cuts the fibrin strands and dissolves the clot, and produces re-perfusion of the occluded vessel.
SAQ/Viva
Describe mechanism of action of streptokinase / Urokinase / r-tPA / Tenecteplase.
All the drugs in the above question are thrombolytics, and obviously have same mechanism of action.
They potentiate/activate the natural thrombolytic system inside the body which consists of tissue plasminogen activator, factor XIIa, and Kallikrein.
SAQ/LAQ/Viva
Mention thrombolytic drugs and their uses.
Thrombolytic drugs include:
- Streptokinase:
- Acts on fibrin bound as well as circulating plasminogen.
- It is obtained from beta hemolytic streptococcus group C culture, and has more incidence of hypersensitivity.
- Streptokinase is given as intravenous infusion.
- Reteplase Alteplase, Anistreplase, Tenecteplase: Are selective on fibrin bound plasminogen.
- They are obtained by recombinant DNA technique from human endothelial cell culture, and hence are non-antigenic.
- Tenecteplase can be given as a single intravenous bolus dose. Others need to be given by intravenous infusion and need to be repeated.
Uses of thrombolytics:
1. Acute myocardial infarction:
Thrombolytics are useful to dissolve the clot and establish re-perfusion of the occluded vessel. They are more effective when given during first 3-4 hours. They reduce the area of necrosis and improve ventricular function. They decrease the mortality.
2. Pulmonary embolism
3. Stroke
4. Peripheral arterial occlusion
5. Arterial catheter occlusion
6. Venous catheter occlusion
7. Deep vein thrombosis