Antihypertensive Drugs
- Antihypertensive drugs are presented in the following three video sessions. Have a brief overview:
Hypertension (what people call BP !) is an important condition responsible for probable complications like heart failure, myocardial ischemia, renal damage, retinopathy, and transient ischemic attacks.
When the increased blood pressure is due to ascertainable causes such as Renal artery stenosis/Renal disease (Renovascular hupertension), Cushing disease/syndrome, Pheochromocytoma, Long-term corticosteroid therapy or such definitive causes, then – it means that this blood pressure is secondary to these causes. Such hypertension is called Secondary Hypertension. It can be also looked upon as organic/structural hypertension.
Whereas when we cannot find any cause for the rising blood pressure, then it is called Essential Hypertension. It can be also called Primary or Functional or Idiopathic. It means the science yet does not know a single, identifiable cause for this phenomenon.
LAQ/SAQ/Viva
Classify Antihypertensive drugs with examples.
There are more groups of antihypertensive agents which are not in much use. They include:
- Adrenergic neurone blockers: Guaethidine
- Catecholamine depleters: Reserpine
- Ganglion blockers: Trimethaphan, Mecamylamine
- 5 HT antagonists: Ketanserin
SAQ/Viva
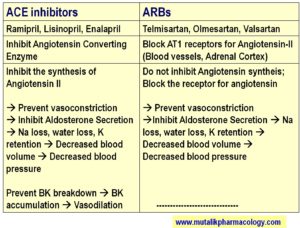
Compare and Contrast: ACE Inhibitors and ARBs (Angiotensin Converting Enzyme Inhibitors and Angiotensin Receptor Blockers)
Below are the tables which differentiate/compare the two groups based on the mechanism of action, and then also on their adverse effects. (Refer to these tables and read the description below the table.)
SAQ/Viva
Explain the mechanism of action of ACE Inhibitors to decrease the blood pressure.
1. ACE-Inhibitors inhibit the enzyme Angiotensin Converting Enzyme. So the conversion of Angiotensin I to Angiotensin II is inhibited. (Angiotensin II is supposed to constrict the blood vessels and increase the blood pressure) Now because Angiotensin II synthesis is inhibited, vasoconstriction will be prevented. This leads to decrease in blood pressure.
2. Since Angiotensin II synthesis is inhibited, it inhibits the Aldosterone secretion from adrenal cortex. (Angiotensin II is supposed to stimulate the adrenal cortex to secrete aldosterone; and aldosterone is supposed to increase the Na and water retention, and increase the blood volume and thereby increase the blood pressure) . Now due to inhibition of aldosterone secretion, Na and water are lost, which leads to excretion of blood volume, and thereby there is decreased in blood pressure.
3. Angiotensin Converting Enzyme (ACE) is same as Kininase II enzyme which is supposed to break down Bradykinin. Due to inhibition of this enzyme, Bradykinin is not broken down, and it accumulates. Bradykinin is a potent vasodilator, and its accumulation leads to decrease in blood pressure.
SAQ/Viva
Classify Calcium channel blockers with examples.
Calcium channel blockers block the L-type calcium channels present in the cardiovascular system. By blocking the calcium channels, the calcium entry is reduced. So there is suppression of the heart and vasodilation in the blood vessels, which leads to fall in blood pressure.
Some of them have more predominant action on blood vessels (drugs ending with dipine: nifedipine, amlodipine etc), so they are said to act on the periphery of circulation (means blood vessels); while Verapamil and Diltiazem are known for their predominant effects on heart, so they are said to act predominantly on center of circulation (means heart). Between the two, verapamil suppresses the heart more as compared to diltiazem.
Calcium channel blockers dilate arterioles as well as venules, but in general dilate the arterioles more predominantly as compared to venules, which is indicated in the following text as A > V,
1. Acting mainly on Blood vessels: (Periphery of circulation)(A>V) (Dilate arterioles more than veins): Di-Hydro-Pyridines: Nifedipine, Amlodipine, Nicardipine, Felodipine
2. Acting predominantly on Heart: (Center of circulation)
Di-Phenyl-Alkyl amine: Verapamil (more negative ionotropic)
Benxo-thiaze-pines: Diltiazem (Less negative ionotropic than verapamil)
LAQ/SAQ/Viva
Mention therapeutic uses and adverse effects of calcium channel blockers.
Adverse effects of calcium channel blockers:
Vasodilation is the key word for Dipines (Nifedipine, Felodipine etc). Due to vasodilation, there is reflex tachycardia, palpitation, throbbing headache, flushing, and sometimes dizziness.
Amlodipine produces least reflex tachycardia.
Dipines are also known to produce ankle edema.
Myocardial suppression is the key word for Verapamil. So it may lead to negative ionotropic effect, bradycardia, hypotension, and AV Block.
Calcium channel blockers can worsen the heart failure or myocardial infarction or AV block.
Verapamil is known to produce constipation and nausea.
Therapeutic uses:
- Hypertension
- Angina – Classical (angina of effort) and Vasospastic angina
- Supraventricular Tachyarrhythmias: Paroxysmal supraventricular tachycardia (PSVT)
- Migraine
- Nocturnal cramps
- Stroke/Subarachnoid hemorrhage (Nimodipine)
SAQ/Viva
Classify direct vasodilators with examples:
(A) Arteriovenular Dilators: Sodium Nitroprusside (arterioles and venules equally), Nitroglycerine (Mainly venodilator)
(B) Arteriolar dilators: Hydralazine, Diazoxide, Minoxidil
SAQ/Viva
Why Sodium Nitroprusside is used in hypertensive crisis? Mention the dose, route of administration, and precautions.
-Sodium Nitroprusside dilates arterioles as well as venules
-It has a rapid onset of action
-It promptly decreases high levels of blood pressure
-It is a potent vasodilator; activates gyanylyl cyclase, increases cGMP, releases nitric oxide, and produces vasodilation
-It decreases preload as well as afterload
Dose: 0.5 mcg/kg/min to begin with, increased if needed upto 10 mcg/kg/min
Route: Continuous intravenous infusion (IV Drip)
Precautions:
-Use freshly prepared solution
-Monitor the blood pressure and adjust the dose
-Cover the infusion bottle with black/brown paper or aluminium foil (because nitroprusside is light sensitive, and may get decomposed on exposure to light)
SAQ/Viva
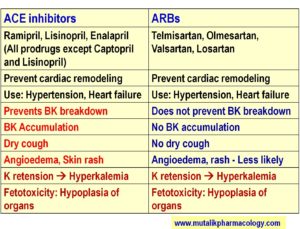
Mention therapeutic uses and adverse effects of ACE inhibitors.
Therapeutic Uses:
- Long-term treatment of Hypertension
- Heart failure
- Myocardial infarction
- To prevent the incidence of sudden death due to Myocardial Infarction or Stroke
- To prevent/delay the renal damage in patients with diabetes (Protective in Diabetic Nephropathy)
- To prevent/delay the renal damage in non-diabetic patients
Adverse Effects:
- Dry Cough: Common adverse effect. ACE inhibitors also inhibit the enzyme Kininase II. So bradykinin breakdown is prevented. Hence Bradykinin accumulates, hence dry cough.
- Hyperkalemia: Increased serum potassium levels. (Aldosterone produces Na retention and K loss. So Inhibition of Aldosterone leads to Na loss and K retention. So hyperkalemia.
- Urticaria and Skin rashes
- Angioedema
- Fetotoxicity: Hypoplasia of various organs / fetal growth retardation / fetal death: Hence ACE inhibitors are contraindicated in pregnancy.
- Dysgeusia: Altered taste sensation. Especially with Captopril. Related to sulfhydryl group in the structure. Less with other ACE inhibitors.
SAQ/Viva
Why ACE Inhibitors produce dry cough and why ARBs (Angiotensin Receptor Blockers) do not produce it?
ACE inhibitors (Captopril, Enalapril, Lisinopril, Ramipril etc..) inhibit the Angiotensin Converting Enzyme (ACE), which converts Angiotensin I to Angiotensin II. This enzyme is from the family of enzymes called Kininase. So ACE is same as Kininase II, which is supposed to breakdown Bradykinin (BK). Since the same enzyme is inhibited, bradykinin breakdown is inhibited. So Bradykinin accumulates in the lungs, and this produces dry cough, as an adverse effect of ACE Inhibitors.
On the other hand, the ARBs (Angiotensin Receptor Blockers – Telmisartan, Losartan, Olmesartan etc..) act further on the Angiotensin Receptor (AT-1 receptor). They do not inhibit the Angiotensin Converting Enzyme or Kininase II. Hence there is no question of inhibiting bradykinin breakdown and bradykinin accumulation. Hence ARBs do not produce dry cough.
Super
Thanks for the compliment.