Antihistamine Drugs or Antihistaminics
The word “Antihistamine drugs or Antihistaminics” has been traditionally used in literature to describe the H1 blockers, which are also called as traditional / classical / conventional antihistamines. These are the drugs that are useful mostly for allergic conditions.
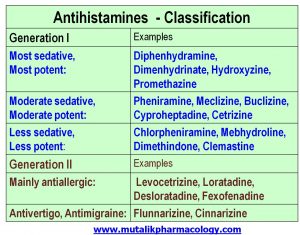
H1 blockers have 2 generations – Generation 1 (like diphenhydramine, hydroxyzine) are older, and they also depress the CNS and produce sedation and disorientation. Generation 2 (like levocetrizine, fexofenadine, loratadine, desloratadine) are newer and less sedating, so they are preferred.
The drugs which block H2 receptors mainly decrease the gastric acid secretion and are usually identified by the name “H2 blockers” such as ranitidine, famotidine etc. They are usually described with the chapters in GIT.
Don’t confuse between H2 blockers and Generation 2 !!!
Special Points:
- Whenever someone says Antihistaminics, it invariably and usually means H1-antihistaminics.
- Classical / Traditional / Conventional antihistaminics means H1-antihistaminics or H1-blockers or H1-receptor antagonists.
- They may be older (Generation I) or newer (Generation II).
- Generation I may produce CNS depression; Generation II are less sedating.
SAQ/Viva
Classify antihistamines with examples.
Antihistamines means H-1 antagonists or H-1 blockers.
They are classified into Generation I (Older/sedating) and Generation II (Newer/Less sedating).
SAQ/LAQ/Viva
Enumerate the pharmacological actions of antihistamines.
Antihistamines competitively block H1 receptors to oppose the allergic manifestations of histamine release. In addition, they block muscarinic receptors, and alpha receptors. Some H-1 blockers also cross the blood brain barrier. Some of them may produce CNS depression, and some may exert anti-migraine and anti-vertigo actions.
1. Antagonism of histamine: Inhibit triple response, histamine induced bronchoconstriction, and smooth muscle contraction.
2. Antiallergic actions: Decrease edema, itching, rash, urticaria, angioedema, and redness.
3. CNS: (CNS depression, antimigraine, antivertigo, anti-motion sickness actions)
- CNS depression,decreased concentration and alertness, diminished motor function, sedation, antianxiety action, drowsiness, disorientation, sleep, disturbed psychomotor function, hypotension
- Antimigraine effect
- Antivertigo effect
- Anti-motion sickness action
4. Anticholinergic actions: Block muscarinic receptors, Decrease secretions, relaxation of smooth muscles
5. Alpha blocking action: This action happens in higher doses, and hence can cause Hypotension when there is overdose of antihistamines.
6. Block 5-HT receptors: Some antihistamines have additional anti-5-HT actions. Produce sedation, increase appetite, decreases itching
7. Antiemetic effect
8. Antitussive effect: Supress cough, decrease secretions
9. Anti-Parkinson action: Related to antimuscarinic effect – useful in drug-induced Parkinson – Decrease tremors, rigidity, sialorrhea
10. Local anesthetic action
LAQ./SAQ/Viva
Mention therapeutic uses of antihistamines.
1. Symptomatic treatment of allergic disorders:
- Allergic rhinitis, conjunctivitis, bronchitis, hay fever, polinosis
- Insect bites, environmental allergies
- Hypersensitivity/allergic reactions to drugs, foods
- Skin diseases – urticaria, eczema, dermatitis, fungal infections
2. Symptomatic treatment of common cold – e.g. Diphenhydramine, chlorpheniramine, pheniramine, levocetrizine, fexofenadine
3. Sympotomatic treatment of cough – e.g Diphenhydramine, chlorpheniramine, pheniramine, levocetrizine
4. Symptomatic relief of vomiting – also for preventing post-operative vomiting and vomiting due to radiation sickness – e.g. promethazine
5. Motion sickness – Prometazine chlorotheophyllinate (Avomine), cyclizine, diphenhydramine, dimenhydrinate etc
6. As sedative, hypnotic, anxiolytic
7. Pre-anesthetic medication: e.g. Promethazine (also for Post-operative vomiting)
8. Drug induced dystonias, drug induced Parkinson (extra pyramidal reactions): Diphenhydramine, cycrimine, procyclidine, biperiden, benzhexol, benztropine (many of these are atropine substitutes).
9. Treatment of vertigo, treatment of Meniere disease: Cinnarizine
10. Treatment of migraine: Flunnarizine
11. Symptomatic relief of severe pruritus (itching) associated with many conditions – e.g. Hydroxyzine
SAQ/Viva
Mention adverse effects of antihistamines.
- CNS depression, drowsiness, sleep, disorientation: More likely with Older antihistamines, because they cross blood brain barrier and produce CNS depression. (Less with 2nd generation antihistamines)
- Disturbance of psychomotor function, motor incoordination, decreased alertness/wakefulness, decreased concentration, impairment of psychomotor performance, leading to serious affection of skillful acts like driving, operating machines or instruments, performing surgical procedures, speaking, writing etc. (Less with 2nd generation antihistamines)
- Synergism/additive effect with other CNS depressants including sedative-hypnotics (benzodiazepeines/barbiturates), narcotic analgesics (morphine like drugs), and alcohol – leading to additive toxicity and serious CNS depression. (Less with 2nd generation antihistamines)
- Anticholinergic adverse effects (muscarinic blockade): Dryness of mouth, eyes, respiratory tract, blurring of vision, increased intraocular pressure, retention of urine, urinary hesitancy, constipation. (Less with 2nd generation antihistamines).
- Long term use increases appetite, and may cause weight gain.
- Larger doses can produce hypotension (alpha blocking action)
- Acute overdose / Poisoning: Leads mainly to anticholinergic adverse effects, hypotension, tremors, and convulsions. Acute overdose is treated with Intravenous sodium bicarbonate and physostigmine/neostigmine. Physostigmine has better penetration across blood brain barrier.
SAQ/Viva
Mention generation 2 antihistamines. Mention the differences between generation 1 and generation 2 antihistamines.
Generation 2 antihistamines:
Mainly used as antiallergic: Levocetrizine, Loratadine, Desloratadine, Fexofenadine
Mainly used as antivertigo, antimigraine: Cinnarizine, Flunnarizine
- Generation 2 antihistamines have less penetration across Blood brain barrier, so there is less marked depression of CNS.
- Less chances of drowsiness, less chances of affecting alertness/wakefulness/motor function/incoordination.
- Less chances of impairment of psychomotor performance and affection of skillful acts. Hence they can be used in persons involved in skillful acts like driving, operating machines, using instruments etc. or can be used during daytime.
- Less chances of producing additive toxicity with other CNS depressant such as other sedative hypnotics (benzodiazepines, barbiturates, narcotic analgesics etc) or alcohol.
- More selectively block H1 receptors.
- Anticholinergic adverse effects (dryness of mouth, retention of urine, blurring of vision etc) are less marked.
- Probable more selective antiallergic action by inhibiting effects of leukotrienes and platelet activating factor
Because when it came to market, they believed it was less sedating, but later its proven to produce moderate sedation.